In recent years, the importance of monitoring vascular health has gained significant attention, particularly as cardiovascular diseases continue to be a leading cause of morbidity worldwide. While clinical assessments remain the gold standard, there is growing interest in developing reliable methods for at-home vascular elasticity testing. These methods empower individuals to track their vascular health proactively, potentially identifying early signs of stiffness or deterioration before serious complications arise.
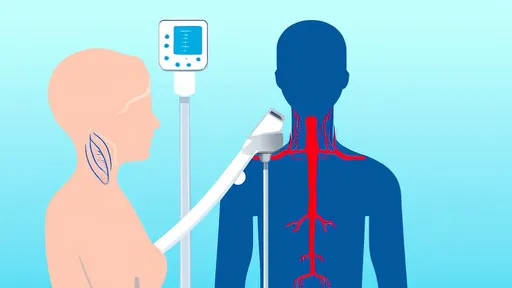
The concept of vascular elasticity revolves around the ability of blood vessels to expand and contract in response to blood flow. Healthy arteries are flexible and resilient, whereas stiffened arteries—often a result of aging, hypertension, or atherosclerosis—can increase the risk of heart attacks and strokes. Traditional methods like pulse wave velocity (PWV) and carotid-femoral assessments require specialized equipment and trained professionals. However, emerging techniques now allow for simplified, non-invasive measurements that can be performed at home with reasonable accuracy.
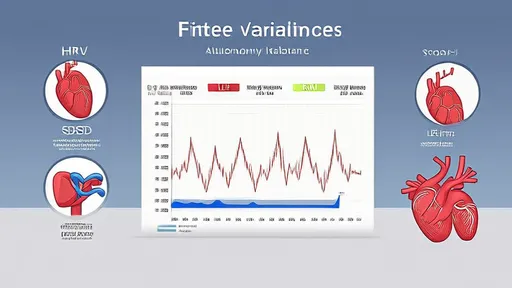
One promising approach involves the use of photoplethysmography (PPG) sensors, commonly found in wearable devices like smartwatches and fitness trackers. These sensors detect blood volume changes in the microvascular bed of tissues, typically through the skin. By analyzing the shape and timing of the pulse wave, algorithms can estimate arterial stiffness. While not as precise as clinical tools, these devices provide a convenient way to monitor trends over time. For instance, a gradual increase in pulse wave amplitude or a shift in waveform morphology may indicate reduced vascular elasticity, prompting further medical evaluation.
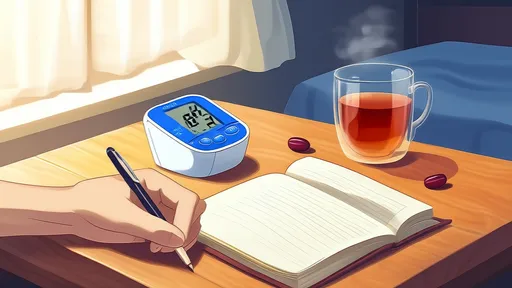
Another method gaining traction is the oscillometric blood pressure-based assessment. Some modern blood pressure monitors now incorporate algorithms that analyze pulse wave characteristics during routine measurements. These devices assess parameters like the augmentation index (AIx), which reflects wave reflections in the arterial tree. Higher AIx values often correlate with increased arterial stiffness. Though these readings should not replace professional diagnostics, they serve as valuable indicators for those managing hypertension or other cardiovascular risk factors.
The rise of smartphone applications further expands possibilities for home-based vascular monitoring. Certain apps utilize the phone’s camera and flashlight to capture fingertip pulse waveforms, similar to PPG technology. Users place their finger over the camera lens, and the app processes the subtle changes in light absorption caused by blood flow. Advanced algorithms then derive metrics related to vascular tone and elasticity. While skepticism remains regarding the accuracy of such methods, studies suggest they can provide meaningful data when used consistently under controlled conditions.
Lifestyle factors play a crucial role in vascular elasticity, and home testing can motivate positive behavioral changes. Regular aerobic exercise, a diet rich in antioxidants, and stress management techniques like meditation have all been shown to improve arterial flexibility. By tracking vascular metrics alongside lifestyle modifications, individuals can observe correlations between their habits and vascular health. For example, someone who starts a daily walking routine might notice gradual improvements in their pulse wave readings, reinforcing the benefits of physical activity.
Despite the advantages, it’s important to acknowledge the limitations of home-based vascular assessments. Variability in measurement conditions—such as body position, hydration levels, or time of day—can influence results. Additionally, these methods are not diagnostic tools but rather screening aids. Abnormal findings should always be followed up with a healthcare provider for comprehensive evaluation. Nevertheless, the ability to monitor vascular trends at home represents a significant step toward personalized preventive care.
As technology advances, the accuracy and accessibility of these tools will likely improve. Researchers are exploring innovations like multi-wavelength PPG sensors and machine learning algorithms to enhance reliability. In the future, integrating home vascular data with electronic health records could enable more dynamic interactions between patients and providers, fostering earlier interventions when needed.
Ultimately, the democratization of vascular health monitoring aligns with broader trends in patient-centered care. By equipping individuals with simple yet insightful tools, we move closer to a paradigm where health is not merely managed reactively but nurtured proactively. Whether through wearables, smart devices, or innovative apps, the power to understand and influence vascular elasticity is increasingly within reach—right from the comfort of home.
By /Jul 14, 2025
By /Jul 14, 2025

By /Jul 14, 2025
By /Jul 14, 2025
By /Jul 14, 2025
By /Jul 14, 2025

By /Jul 14, 2025

By /Jul 14, 2025

By /Jul 14, 2025
By /Jul 14, 2025

By /Jul 14, 2025

By /Jul 14, 2025

By /Jul 14, 2025

By /Jul 14, 2025

By /Jul 14, 2025

By /Jul 14, 2025

By /Jul 14, 2025
By /Jul 14, 2025
By /Jul 14, 2025
By /Jul 14, 2025