The growing prevalence of non-alcoholic fatty liver disease (NAFLD) has spurred intense research into novel therapeutic approaches, particularly those targeting the gut-liver axis. As the scientific community delves deeper into the intricate relationship between gut microbiota, intestinal permeability, and hepatic metabolism, a new frontier of intervention strategies is emerging. These approaches aim to modulate the gut environment to indirectly improve liver health, offering hope for millions affected by this silent epidemic.
Gut Microbiota Dysbiosis: A Key Player in NAFLD Pathogenesis
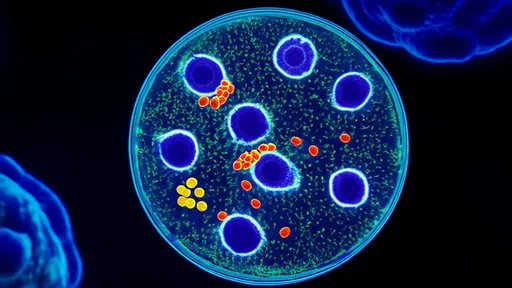
Emerging evidence paints a compelling picture of gut microbiota's role in NAFLD development and progression. The microbial communities residing in our intestines do far more than aid digestion - they actively participate in regulating metabolic processes that directly impact liver function. Studies reveal distinct microbial signatures in NAFLD patients, characterized by reduced microbial diversity and overrepresentation of pro-inflammatory species. These dysbiotic patterns correlate with increased intestinal production of lipopolysaccharides (LPS) and other microbial metabolites that promote hepatic inflammation and insulin resistance.
The gut-liver axis operates as a bidirectional communication highway, with microbial-derived signals traveling through the portal vein to influence hepatic metabolism. Certain bacterial species, such as those producing trimethylamine N-oxide (TMAO), have been implicated in exacerbating hepatic steatosis. Conversely, bacteria that generate short-chain fatty acids (SCFAs) like butyrate appear protective, enhancing gut barrier function and reducing systemic inflammation. This microbial imbalance creates a perfect storm for NAFLD progression, making microbiota modulation an attractive therapeutic target.
Intestinal Barrier Dysfunction: The Leaky Gut Connection
Beyond microbial composition, the physical integrity of the intestinal barrier plays a crucial role in NAFLD pathophysiology. A compromised gut barrier, often referred to as "leaky gut," allows translocation of bacterial products and dietary antigens into portal circulation. This breach triggers a cascade of inflammatory events that ultimately reach the liver, where Kupffer cells become activated and initiate local inflammatory responses.
Zonulin, a protein that regulates tight junction permeability, has emerged as a biomarker for intestinal barrier dysfunction in NAFLD. Elevated serum zonulin levels correlate with disease severity, suggesting that therapeutic strategies aimed at tightening these junctions could yield clinical benefits. Interestingly, certain dietary components like gluten can stimulate zonulin release, hinting at potential dietary modifications that might support gut barrier integrity.
Bile Acid Metabolism: A Microbial-Hepatic Dialogue
The intricate dance between gut microbes and bile acid metabolism represents another promising intervention point. Gut bacteria extensively modify primary bile acids into secondary forms, creating a diverse pool of signaling molecules that influence both hepatic and systemic metabolism. These modified bile acids activate nuclear receptors like FXR and TGR5, which regulate glucose homeostasis, lipid metabolism, and energy expenditure.
In NAFLD, this delicate balance becomes disrupted, with alterations in bile acid composition and signaling contributing to metabolic dysfunction. Therapeutic approaches that restore healthy bile acid profiles - whether through microbial manipulation, bile acid sequestrants, or FXR agonists - show considerable promise. The recent approval of obeticholic acid, an FXR agonist, for certain liver conditions underscores the therapeutic potential of targeting this pathway.
Gut-Derived Metabolites: The Molecular Messengers
The gut microbiota generates a vast array of metabolites that profoundly influence hepatic health. Beyond SCFAs and bile acids, other microbial products like indole derivatives, phenolic compounds, and various amino acid metabolites participate in complex metabolic cross-talk with the liver. These molecules can modulate hepatic lipid accumulation, oxidative stress, and inflammatory responses through multiple mechanisms.
For instance, indole-3-propionic acid, a tryptophan metabolite produced by certain gut bacteria, has demonstrated protective effects against hepatic steatosis in preclinical models. Similarly, microbial metabolism of dietary choline and carnitine influences hepatic very-low-density lipoprotein (VLDL) secretion and lipid partitioning. Understanding these intricate metabolic networks opens doors to precision interventions targeting specific microbial pathways.
Emerging Intervention Strategies
Therapeutic exploration in this field spans multiple approaches, from dietary modifications to pharmacologic agents and microbial transplantation. Mediterranean-style diets rich in polyphenols consistently demonstrate benefits for both gut health and NAFLD parameters, likely through their prebiotic effects and anti-inflammatory properties. Specific fibers like resistant starch and inulin show particular promise in selectively nourishing beneficial gut bacteria.
Probiotic supplementation, especially with strains like Lactobacillus and Bifidobacterium species, has yielded modest but consistent improvements in liver enzymes and markers of hepatic steatosis. More radical approaches like fecal microbiota transplantation (FMT) are currently under investigation, with early trials showing intriguing results in metabolic parameters. Meanwhile, pharmacologic agents that target gut-derived molecules, such as endotoxin inhibitors and bile acid modulators, continue to advance through clinical development pipelines.
Challenges and Future Directions
Despite these promising developments, significant challenges remain in translating gut-targeted approaches into clinical practice. The incredible interpersonal variability in gut microbiota composition complicates the development of universal interventions. Personalized approaches that consider an individual's microbial fingerprint may eventually prove necessary for optimal outcomes.
Long-term safety concerns, particularly with approaches like FMT, require thorough investigation. Additionally, our understanding of the complex interactions between diet, microbiota, and host metabolism remains incomplete. Future research must focus on elucidating causal relationships rather than mere associations, employing sophisticated multi-omics approaches and well-designed intervention trials.
The gut-liver axis represents a paradigm shift in our understanding and treatment of NAFLD. As we continue to unravel the complex dialogues between our microbial inhabitants and hepatic metabolism, novel therapeutic opportunities will undoubtedly emerge. While much work remains, targeting the gut ecosystem offers a promising avenue for addressing this increasingly prevalent metabolic disorder at its roots.
By /Jul 14, 2025
By /Jul 14, 2025

By /Jul 14, 2025
By /Jul 14, 2025
By /Jul 14, 2025
By /Jul 14, 2025

By /Jul 14, 2025

By /Jul 14, 2025

By /Jul 14, 2025
By /Jul 14, 2025

By /Jul 14, 2025

By /Jul 14, 2025

By /Jul 14, 2025

By /Jul 14, 2025

By /Jul 14, 2025

By /Jul 14, 2025

By /Jul 14, 2025
By /Jul 14, 2025
By /Jul 14, 2025
By /Jul 14, 2025